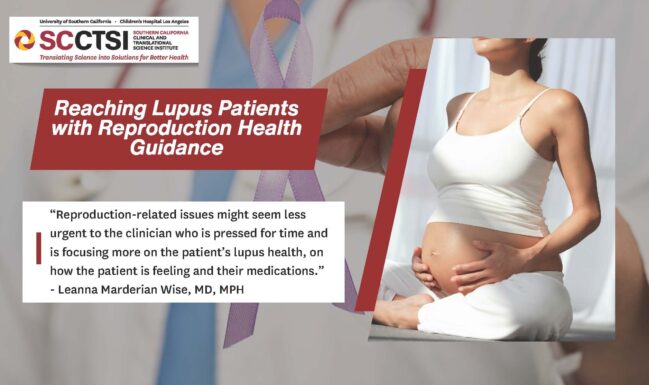
Reaching Lupus Patients with Reproductive Health Guidance
A SC CTSI biostatistician helped researchers identify disparities in clinician-patient communications about lupus and reproductive health.
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease that predominantly affects women of childbearing age. Lupus occurs in greater incidence and severity in Spanish speakers, who also have higher rates of unplanned pregnancies compared with non-Hispanic whites.
Some medications prescribed to treat lupus can cause birth defects or developmental malformations in a fetus after exposure during pregnancy.
“You can have a healthy pregnancy with lupus, but you have to do it carefully,” said Leanna Marderian Wise, MD, MPH, assistant professor of clinical medicine at the Keck School of Medicine at the University of Southern California (USC). “You need the right regimen and have the disease under control for the best results.”
Doctors caring for female lupus patients should more consistently query them about pregnancy plans, contraception, and medication use.
“You’d rather not have these patients show up to the ER when four months pregnant,” said Wise.
Yet Spanish-speaking lupus patients receiving treatment at a Los Angeles rheumatology clinic were less likely to have discussions with their doctors about reproductive health than English-speaking patients, according to a study led by Wise and published in the journal Lupus Science and Medicine.
The study team included Jack Rodman, MPH, a biostatistician with the Southern California Clinical and Translational Science Institute (SC CTSI), who helped refine the patient survey, wrote the methods section and responded to peer reviewers' statistical questions.
The Wise study surveyed 151 female lupus outpatients at the Los Angeles General Medical Center (LAGMC), the largest safety net hospital in Los Angeles, which is affiliated with USC. Patients could choose the English or Spanish language survey.
All survey participants were asked whether their lupus doctor initiated at least one discussion regarding contraception in the past year. In the English-speaking survey, 72.6% of respondents affirmed that their lupus doctor did have this conversation with them. Only 29.5% in the Spanish language survey affirmed that their doctors had done so.
Another survey question was whether lupus doctors asked about pregnancy plans for the upcoming year. In the English-speaking survey, 73.8% responded in the affirmative that their doctor did raise this question, in contrast to 45.3% who took the Spanish survey.
These disparities could be driven partly by language barriers, which add complexity and take up valuable time during a visit, despite aid from translators or translation services, Wise noted.
“Reproduction-related issues might seem less urgent to the clinician who is pressed for time and is focusing more on the patient’s lupus health, on how the patient is feeling and their medications,” Wise added. “It could be the clinician thinking, ‘I will just save contraception or pregnancy planning for another visit.’”
One question from peer reviewers was whether the difference in average patient age between the two populations could explain disparities in communication with their doctors. Spanish speakers in the study were older on average, though still of child-bearing age.
“When the reviewers wanted more details about the impact of age, Jack Rodman of SC CTSI, as our biostatistics expert on the paper, was very responsive,” Wise said. “Jack’s analysis showed that clinicians are not counseling Spanish-speaking women as effectively as English-speaking patients, even when adjusting for age. Sometimes people delay their families because of lupus. Even if Spanish speakers are a little older, you still need to ask the important questions.”
Rodman found the experience of collaborating with Dr. Wise fruitful as well, especially in light of the findings.
“Being a part of this project with Dr. Wise has been incredibly rewarding and has highlighted the discrepancies many non-English speaking patients may face in a healthcare setting. This is particularly important at the intersection of reproductive health and disease management, which was the focus of this study,” Rodman said. “Working with Dr. Wise has also shown the benefits of creating an early partnership between investigators and Biostatisticians. We encourage clinician-researchers, particularly junior faculty, to engage with BERD group members as early as possible to get the most assistance regarding study design and developing an analysis plan.”
This study did not answer why these disparities in reproductive health discussions are so significant between the two patient populations. Wise’s plan for the next stage of this research effort will address that question.
“I’m hoping to use this study for foundational data, generating a hypothesis and exploring that question in a larger study,” she said.
Wise also encouraged other young physician-scientists to collaborate with staff of the SC CTSI Biostatistics, Epidemiology and Research Design (BERD) Core Group.
“You can request free hours for each part of your research project from BERD as long as you are junior faculty,” she said. “You can request free hours in each phase—as you conceive your project, analyze data and then respond to reviewers.”