SC CTSI-Supported Research Finds Kids with Tracheostomies Have High Rate of Hospital Readmission
The team led by Christopher Russell, MD, hopes to develop evidence-based guidelines for prevention, diagnosis and treatment of respiratory infections in pediatric patients with tracheostomy.
Dr. Christopher Russell is an SC CTSI research scholar alum received support from the SC CTSI Biostatistics, Epidemiology, and Study Design (BERD) program.
Christopher Russell, MD, a hospitalist at Children’s Hospital Los Angeles specializing in pediatric patients with tracheostomies, noticed that many of these children have a high percentage of being re-admitted to the hospital for respiratory conditions. A tracheostomy is a surgical opening created in the airway during a tracheotomy procedure to help patients who are unable to breathe on their own.

What could doctors be doing better for these patients? Russell hoped to find clinical guidelines on the management of respiratory infections for this population, but his search through the literature yielded little results. He found there were very few studies.

Christopher Russell, MD
“The goal of my research is really to develop evidence-based guidelines for prevention, diagnosis and treatment of respiratory infections in pediatric patients with tracheostomy,” explained Russell.
He was moved to conduct a multicenter, retrospective study of more than 4,000 patients at 48 children’s hospitals (all part of the Children’s Hospital Association) across the country to learn about treatments and health outcomes of these patients. He really wanted to understand the possible variations of hospital-level care such as diagnostics, antibiotic therapies, and how these affect the patients’ length of stay and likelihood of readmission in children with tracheostomies hospitalized for bacterial respiratory tract infections.
What he found was that there was a lot of variety in the care kids are given at all hospitals and that the rate of readmission remains high across all of the pediatric hospitals included in the study. Overall, the 30 day revisit rate was almost 30 percent. The research findings were published in the journal Hospital Pediatrics in a paper titled “Care Variations and Outcomes for Children Hospitalized With Bacterial Tracheostomy-Associated Respiratory Infections.”
Russell and co-authors, Wendy J. Mack, PhD, Sheree M. Schrager, PhD, MS, and Susan Wu, MD, concluded that future research should focus on standardizing the diagnosis and treatment of children with tracheostomies to prevent readmission to the hospital for this population.
“As a hospitalist at CHLA, I treat kids, but my goal is to keep kids out of the hospital, if I can,” said Russell. “If we can find a way to minimize kids’ needs to come to the hospital or find ways to stabilize them more quickly and send them home, that would be ideal.”
Because of the large number of children who undergo tracheotomy procedures at CHLA, Russell and his colleagues saw an opportunity to further investigate the risk factors for bacterial tracheostomy-associated respiratory tract infections that required hospital readmission. Identifying high-risk populations and developing evidence-based best practices for the prevention and treatment of respiratory infections like Pseudomonas aeruginosa – an antibiotic-resistant bacterium – could reduce the hospital readmissions. The results of their new study – published online in the journal Pediatric Pulmonology – demonstrates that among pediatric patients who undergo tracheotomy, those of Hispanic ethnicity and those who acquire Pseudomonas aeruginosa after the procedure and before discharge are at increased risk of being readmitted for a bacterial respiratory infection.
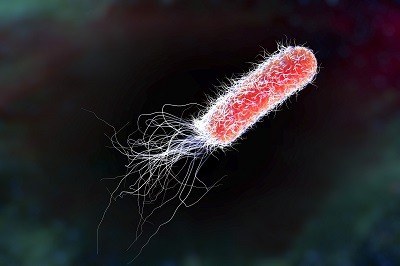
Bacterium Pseudomonas aeruginosa, an antibiotic-resistant nosocomial bacterium.
Results showing poorer outcomes in Hispanic patients are consistent with past literature demonstrating health care disparities in Hispanics. Further, Hispanic ethnicity is associated with higher mortality rate in patients with other respiratory diseases such as cystic fibrosis, and in those undergoing surgical procedures such as congenital heart surgery repair. The poorer outcomes may be due to biological differences, socioeconomic differences including access to care and language difficulties, decreased use of home health services and post-acute facilities or a combination.
Dr. Russell plans to use this data to obtain additional funding to study the role of Pseudomonas aeruginosa in pediatric tracheostomy-associated respiratory tract infections and to examine new diagnostic and treatment options for Pseudomonas respiratory infections.
Other contributors to the paper include Tamara D. Simon, MD, MSPH, Mary R. Mamey, PhD, Christopher J. L. Newth, MD, and Michael N. Neely, MD, MS.
Original article found here.
Images courtesy of Shutterstock.com