SC CTSI-Supported Researchers Create Higher Resolutions of the Brain
Two researchers are developing new MRI protocols to get better images of tumors.
Note: Researchers Krishna Nayak and Meng Law are part of a multi-disciplinary team that received support from the SC CTSI Pilot Funding program to develop new MRI protocols.
Nearly 700,000 people in the United States are living with a brain tumor, and the best way to image most types of these tumors is with magnetic resonance imaging, which use magnetic fields and radio waves to create detailed pictures of the brain.
With current MRI protocols, there is a trade-off between resolution and spatial coverage — that is, one must decide between looking at a large section of the brain in less detail or focusing on a smaller volume in greater detail.
Krishna Nayak, a USC Viterbi School of Engineering professor, is working with neuroradiologist Meng Law to create higher-resolution images of greater portions of the brain than was previously possible.
The way Nayak and his team achieved this goal is somewhat counterintuitive: to get more detailed images, they capture less data with each MRI scan. Then their computer programs use compressibility of the data to create higher-resolution images.
So nothing is missed
For patients and their doctors, the new technology will have an impact.
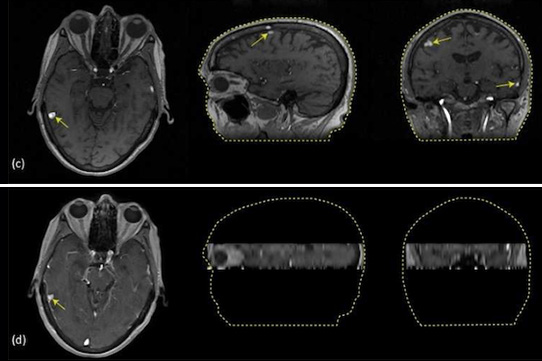
Only four lesions of a patient with metastatic melanoma were captured by the current clinical scan (bottom), but 14 lesions were captured by Krishna Nayak’s experimental scan (top). (Courtesy of Krishna Nayak)
The patient experience will be nearly identical: The scan will take the same amount of time — about five to six minutes — though the machine will make a different sound than the current methods. And for doctors, the resulting images of the brain will be crisper and will cover the entire brain, which is very important if there are multiple small metastases or a single very large tumor.
“It will ensure that nothing is missed,” Nayak said.
On the images shown, bright areas show signs of cancer. The brightness comes from a contrast agent that is injected into the patient just before the scan is performed. The agent is a large molecule — in this case with an atom of gadolinium that is too large to cross the blood-brain barrier unless there is something wrong, such as the growth of a tumor.
The technology could also be used for other conditions that are marked by a breakdown of the blood-brain barrier, such as multiple sclerosis and Alzheimer’s disease. And with this successful clinical test under his belt, Nayak plans to move forward to hone the technology and user-interface for radiology technicians to use this method in more patients, facilitate regulatory approval and make an impact on patient’s lives as soon as possible.
Top priority
“What excites me is that we have a chance to help patients and possibly soon,” Nayak said. “Our immediate goal is to clinically translate this technology for the brain, but it can be applied to other organs as well.”
“Eventually, we will be able to scan the entire human body in a matter of minutes and obtain a lot of imaging information, perhaps even one day molecular and genetic information,” Law added. “This will move health care into the realm of personalized medicine, so that diagnosis and therapeutics [so-called “diapeutics”] can be individualized for each person.”
Other research contributors included Yi Guo and Yinghua Zhu, USC Viterbi Ph.D. candidates in electrical engineering; Sajan Lingala, USC Viterbi postdoctoral research associate; Marc Lebel, a former postdoctoral student currently at GE Healthcare; and Mark Shiroishi, neuroradiologist at Keck Medicine of USC.