Cross-Institutional Study Looks within Arteries To Understand Effects Of Cholesterol Medications
Helping doctors tailor cholesterol medications to lower incidence of heart attack and stroke.
Researchers in a multi-year study are using magnetic resonance imaging (MRI) to understand the long-term effect of statin drugs on the arterial blockages associated with atherosclerosis, the world's leading cause of death and disability.
Patrick Colletti, MD, a professor of radiology at USC and chief of Magnetic Resonance Imaging at LAC+USC Medical Center, launched the six-year project, supported in part by SC CTSI funding and one of SC CTSI's Clinical Trials Units (CTU).

Patrick Colletti, MD
The investigators are imaging the carotid arteries of atherosclerosis patients to compare the impact of a variety of cholesterol medications on fatty deposits called plaques that narrow and block arteries. But not all plaques are equally dangerous, so researchers are using MRI's unique ability to reveal differences in plaque composition and behavior in an effort to determine what health risks individual blockages present, and how best to treat them.
Atherosclerosis is responsible annually for millions of heart attacks, stroke, blood clots, and other medical problems.
Finding the right statin for the job
Because of their ability to both lower cholesterol and shrink plaques, statins have become some of the most-prescribed medications in history. But much remains unknown about the responses of different types of plaques to the various types of drugs currently available.
It is not clear, for example, why some patients experience cardiovascular problems despite their use of statins and consequent reductions in cholesterol levels and plaque size, said Colletti.
Initially, explained Colletti, investigators hope to learn how plaques in the participants' arteries respond to various statins, and to better understand the relationship between medications and the health risks related to atherosclerosis.
Eventually, researchers hope simple MRI scans will be able to give doctors the information they need to tailor therapeutic intervention for individual atherosclerosis patients.
"We'd like to understand which cholesterol-lowering drugs and combinations of drugs to use for any given patient, based on what we know about the plaques in their arteries," said Colletti.
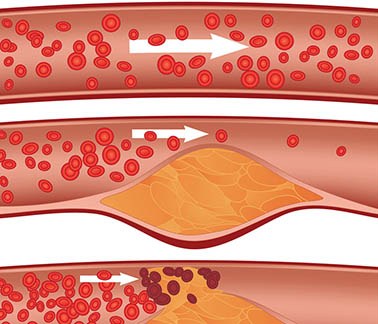
Cholesterol plaque in artery (atherosclerosis): Top artery is healthy. Middle & bottom arteries show plaque formation, rupturing, clotting & blood flow occlusion. (Credit: Diamond Images, shutterstock)
Tracking artery health with MRI scans
For this study, the investigators enrolled 80 adults with atherosclerosis. The research participants were randomly split into three groups. Each group is being treated with one of three regimens of FDA-approved cholesterol lowering therapy, all of which contain the widely prescribed statin medication Lipitor.
At the start of their participation, the researchers scan the carotid arteries of all patients by MRI, and again at yearly intervals, to monitor the development of plaque deposits. After an initial three years of tracking, researchers will ask participants to take part in another three-year series of annual MRI scans, for a total of six years.
Enrolling 80 qualified participants in the study was itself an important success: more than 80% of clinical studies fail because they can't find a sufficient number of research subjects.
"It's always difficult to recruit and retain participants in long-term studies of this nature," said Colletti. But there were surprising rewards to the research: for example, researchers found that one of their newly recruited participants had dangerously high blood pressure. They directed the participant to a clinic, where doctors got her hypertension under control. The research team members were gratified to see that participant's overall health improve dramatically, Colletti said.
The critical question: Are the plaques stable – or not?
Atherosclerosis researchers have long known that not all plaques are alike, explained Colletti. Some are relatively stable and asymptomatic. These plaques are less likely to throw off the tiny particles that can cause blood clots – one of the biggest dangers of atherosclerosis.
But some plaques are less stable and trigger higher levels of inflammation. They are more likely to rupture, shedding particles that can stick to blood platelets, creating the clots that can suddenly and disastrously block blood flow. When these thromboses occur in coronary arteries, heart attacks and other problems can result. In the brain, clots can cause strokes.
Prior to the launch of the carotid plaque study, Colletti had been investigating cardiac MRI when he met MRI researcher Zhao Xue-Qiao, MD, a professor at the University of Washington School of Medicine in Seattle, where she is director of the Coronary Atherosclerosis Research Laboratory.
Since USC has similar research MRI capabilities, the two decided to expand Zhao's carotid plaque composition project to USC. The University of Washington research team will also recruit and examine participants, and will serve as the core site for the analysis of all the carotid MRI scans.

Zhao Xue-Qiao, MD
Spotting dangerous plaques with MRI
The study of atherosclerosis has been revolutionized by MRI, said Zhao. Older x-ray based imaging methods, such as angiography, revealed the size of plaques, but are not capable of providing information about the make-up of the deposits the way MRI can.
"For years we didn't have a good imaging modality to look at arterial plaques in vivo in a non-invasive way," said Zhao. "Now with MRI, we're able to see not just the size of the plaque, but its composition and the level of inflammation."
Over time, MRI scans can show lipids depositing in arteries to form a new plaque, as well as the healing period called fibrosis, and finally calcification, when plaques are less dangerous, said Colletti. This knowledge should enable doctors to determine therapy accordingly.
"We're collecting an increasing body of evidence of how plaques respond to treatment," said Colletti. "Ultimately, we're hoping to use this imaging to predict which plaques are going to be stable for the long-term and which patients will need more aggressive or different forms of therapy to reduce their risk of clinical events."
In addition to funding, the SC CTSI is also supporting the project in another concrete way: by providing an appropriately outfitted facility for Colletti's team to meet and examine research participants. Investigators are conducting part of the study at one of SC CTSI's Clinical Trials Units (CTU). The units provide clinical infrastructure, laboratory and nursing services and support outpatient as well as inpatient research ensuring the compliance with local and federal regulations.
"It's possible to conduct the research in the clinic, but it's much harder," said Colletti. "The CTU provides a stable space for us to conduct this work efficiently."
More information about atherosclerosis can be found at the American Heart Association, a physician-authored resource for evidence-based clinical information.
SC CTSI is part of the 62-member Clinical and Translational Science Awards (CTSA) network funded through the National Center for Advancing Translational Sciences (NCATS) at the NIH (Grant Number UL1TR000130). Under the mandate of “Translating Science into Solutions for Better Health,” SC CTSI provides a wide range of resources, services, funding, and education for researchers and promotes online collaboration tools such as USC Profiles.



