Making Sense of Big Data: USC Biostatistician Helps Lead Research to Identify Increased Stroke Risk in Aortic Repair Surgeries
Li Ding, MD, MPH, a biostatistician at the SC CTSI, worked on a retrospective analysis of thousands of patients whose outcomes were recorded in a national patient registry. The study could help vascular surgeons better protect patients from the risk of stroke during endovascular aortic repair procedures.
To carry out complex repairs to the aorta, the body's largest artery, surgeons frequently conduct their work endovascularly, inserting tools through one or more of a few typical access points in arteries throughout the upper and lower body, and threading them through the blood vessels to the target area. The various arterial entry points offer surgeons different angles and access to the damage they seek to repair.
However, experts do not fully understand the relative risks of the various approaches—specifically for stroke, the most feared and dangerous complication in these aortic procedures. To address this issue, a research team of biostatisticians and vascular surgeons from USC and other institutions dug into a trove of data about patient outcomes collected through a nationwide program called the Vascular Quality Initiative (VQI).
Their retrospective study, an analysis of outcomes involving a subset of approximately 11,600 of the patients in the VQI data, suggested important differences in the risks associated with the various entry points and approaches that may eventually lead to improved guidelines to help surgeons better protect their patients from stroke.
The research team's findings are described in their recent article, "Association of upper extremity and neck access with stroke in endovascular aortic repair," published this year in the Journal of Vascular Surgery.
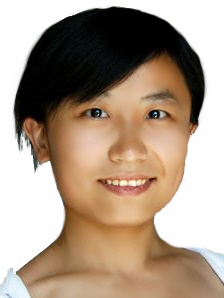
Li Ding, MD, MPH, is a biostatistician in the Biostatistics, Epidemiology and Research Design core group of the Southern California Clinical and Translational Science Institute (SC CTSI). She played a central role in the research, including study design, data analysis, and manuscript of the study.
"In these complex aortic repairs, endovascular surgeons commonly use access points in the upper extremities and the neck," said Ding. "The major question we wanted to address is the differences between those access points. Our hypothesis was that the points in the upper extremities carry a higher stroke risk compared to access points in the lower extremities."
The VQI is a valuable source of data about aortic repair procedures and outcomes. It is a program of the Society for Vascular Surgery, and contains demographic, clinical, procedural and outcome data from more than 700,000 vascular procedures that have been performed at 676 participating medical centers in the United States and Canada. It is designed to help improve care and enable research studies.
The study team sifted through the VQI data to compare patients who had undergone aortic repair procedures that involved arterial access points in the upper extremities such as the arteries of the arm and neck, with patients that had operations relying solely on access through the lower extremities, specifically the iliofemoral artery in the pelvic area. They found that patients who had undergone procedures using arm and neck access faced a substantial two-fold higher risk of stroke compared with patients who had undergone procedures using femoral or iliac-only access.
The large sample size enabled by the VQI dataset conferred particularly strong statistical power in a question of risk that has not been extensively studied, explained Ding. In fact, the new study contradicted a previous, smaller study with a sample size of only 152, which suggested no difference in risk between upper and lower extremity access. But with a sample size of thousands, the VQI-based study, controlling for multiple factors, showed a very clear difference.
"Using the VQI, we were also able to detect the difference between using and multiple upper extremity access, where we found a much higher, three-fold risk of stroke in procedures using multiple access," said Ding. "Future studies may also consider focusing on this question of single versus multiple access."
As valuable as it is, the VQI data can present challenges for researchers conducting retrospective studies, explained Ding. The doctors who contribute outcome and other data to the index do not always follow the same format or record the same type of information. As a result, researchers had to assess the clinical data to determine the specific procedures and other variables associated with each patient. However, Ding's prior training and qualification as a medical doctor helped her work with vascular surgeons on the study team to translate the clinical data in the VQI into data that could be included in the statistical analysis.
Despite the significant findings in terms of the risk of stroke, the team's retrospective analysis is far from the last word on the topic. "This is more like step one," said Ding. "It's telling us that something interesting is happening."
This retrospective analysis will help point the way for future research into aortic repair procedures, said Ding. "The first step is using a national dataset to see and isolate the risk factors, but maybe later on someone can do additional research, such as a clinical trial that looks at specific variables," she said.
Coauthors on the study along with Ding were Anastasia Plotkin, MD; Sukgu M. Han, MD, MS; Gustavo S. Oderich, MD; Benjamin W. Starnes, MD; Jason T. Lee, MD; Mahmoud B. Malas, MD, Fred A. Weaver, MD, MMM; and Gregory A. Magee, MD, MSc.