New Approaches in Online Education for Physicians Who Handle Pediatric Emergencies
Researchers at USC and CHLA collaborate in a multi-institutional study to help train physicians who care for the smallest emergency patients.
Emergency department physicians routinely face difficult medical challenges, but many say that the scariest patient they can imagine is a crashing infant or child.
That's why a team of researchers, including principal investigators at USC and Children's Hospital Los Angeles (CHLA), is developing a new approach to medical education. Their goal is to ensure that emergency department practitioners get all the knowledge they need to deal with pediatric emergencies, through creation of a standardized national curriculum that leverages the reach and flexibility of the internet.
Children and babies make up about 10 percent of emergency cases, but the great majority of them are seen by physicians who are not actually specialists in pediatric emergency medicine (PEM). Most child emergencies are handled by physicians trained in standard (adult) emergency medicine, pediatrics or family medicine.
Although PEM is one of the fastest-growing fellowships in the country, it remains a niche specialty. And many smaller hospitals cannot justify hiring a pediatric emergency specialist.
As a result, non-PEM specialists need additional medical education about pediatric emergency protocols, explained Todd Chang, MD, assistant professor of pediatrics at USC and associate fellowship director in pediatric emergency medicine at CHLA.
Getting everyone on the same page
Individual institutions have addressed this need with coursework of their own, but no standard, national curriculum for non-PEM students had ever been developed. Last year, Chang and co-investigators from CHLA and three other institutions around the country set out to create one.
"There is a certain amount of variation in treatment protocols from hospital to hospital," said Chang. "But our feeling was, 'why can't everyone just learn from the same material?' After all, a fracture in Los Angeles is the same as a fracture in Cincinnati."
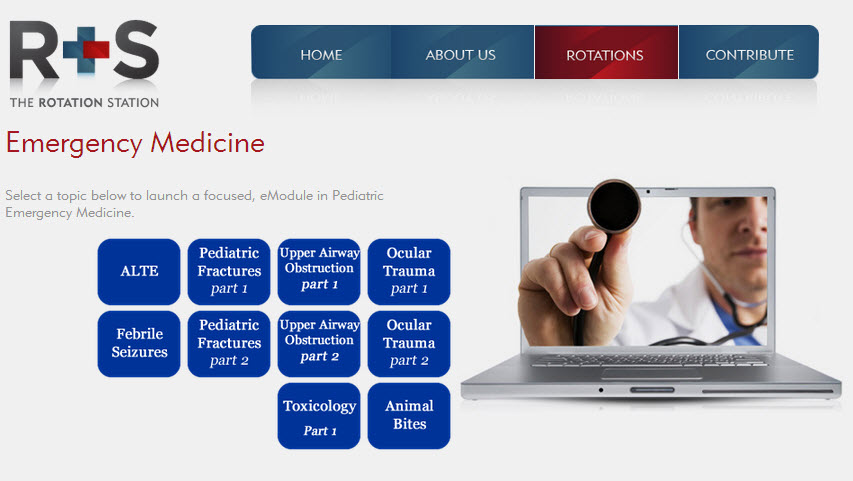
Because their standardized curriculum – called PRELIM (Pediatric Resident Emergency-Medicine Learning & Instructional Modules) – would have to address a uniquely varied student population, investigators decided against a one-size-fits-all set of lectures.
"People come in these courses with extraordinarily different experiences and work styles, so it's impossible to teach them all under traditional lecture hall methods without going over material parts of the class will already know," said Chang.
So they skipped the lectures altogether, and turned to a flexible, internet-based teaching approach. "With online access, everyone can access the same course material, but they can focus on the areas where they need additional training," said Chang.
Investigators tested PRELIM's mini-curriculum with more than 450 study participants from four research centers: CHLA, Children’s National Medical Center at George Washington University in Washington, D.C., Cincinnati Children’s Hospital and Medical Center at University of Cincinnati, and Texas Children’s Hospital at Baylor University, in Houston.
Researchers' initial findings indicate that PRELIM's online education does indeed improve knowledge beyond the rotational experience trainees receive in pediatric emergency departments. Next, investigators plan to expand the study with additional educational modules and more students.
Managing data in the cloud
Internet-based tools were also a key element of the investigators' approach to research data management. With several hundred participants between four institutions, all surveyed multiple times, PRELIM investigators needed to collect and handle large quantities of data efficiently and securely.
They turned to the Research Electronic Data Capture system, called REDCap, a free, secure, HIPAA-compliant, web-based application designed to help scientists rapidly develop databases and surveys for research studies.
Fully vetted by the NIH and many institutional review boards, REDCap comprises more than 900 institutions in 74 countries around the world. At USC and CHLA, REDCap is managed by the Southern California Clinical and Translational Science Institute (SC CTSI).
The strength of REDCap is its ubiquitous access, particularly important for a study that surveyed medical residents, who commonly worked late-night hours.
"Having a cloud-based database and calendar and randomization scheme at a moment's reach through REDCap was immensely helpful," said Chang.
PRELIM co-investigators included Nazreen Jamal, MD, Ted Brenkert, MD, Cara B. Doughty, MD, MEd, Karen Y. Kwan, MD, Kim Little, MD, David J. Mathison, MD, MBA, Phung Pham, MS, and Brad Sobolewski, MD.