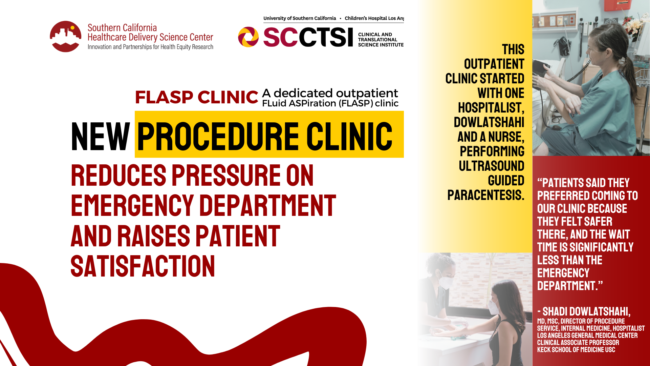
New procedure clinic reduces pressure on emergency department and raises patient satisfaction
An SC CTSI-supported study evaluated an innovative new procedure clinic in Los Angeles for predominately low-income Latino outpatients with cirrhosis, and its success is lessening demand on the emergency department an urban, safety-net hospital.
Cirrhosis of the liver has risen 1.5 to 2 times in the past two decades in the U.S with over 56,000 deaths annually. Among the serious complications of cirrhosis is the painful accumulation of large amounts of fluid in the abdomen, called ascites. Ascites can be relieved by paracentesis, a procedure that drains some of this fluid from the abdomen, but the fluid reaccumulates rapidly. Other more permanent options for management of ascites include the transjugular intrahepatic portosystemic shunt (TIPS) procedure for portal hypertension and liver transplantation. However, low-income communities face significant challenges to receipt of these interventions.
Consequently, low-income patients frequently rely on emergency departments to perform paracenteses—but the repeated need for this procedure burdens clinicians, staff, and the patients themselves, who can wait many hours for this care. Public health crises force the development of an innovative alternative for this care to allow emergency departments to meet the greatly increased demand for urgent care.
“During the COVID pandemic, patients repeatedly returning for paracentesis became a severe challenge for Los Angeles General Hospital, which is a large safety-net hospital serving a predominately low-income Latino population,” said Barbara J. Turner, MD, MSEd, MA, MACP, Professor of Clinical Medicine at Keck School of Medicine of USC. Turner is the lead author of a study recently published in the Journal of General Internal Medicine.
As defined by the Institute of Medicine, a safety net hospital serves primarily patients with Medicaid or no insurance. Financial and staffing barriers in these hospitals commonly prevent outpatient paracentesis from being performed by interventional radiologists. To reduce demand on the emergency department at Los Angeles General Medical Center, Shadi Dowlatshahi, MD, MSc, Director of Procedure Services at LA General and co-author of the study, launched the outpatient FLuidASPiration (FLASP) clinic in March 2021. This outpatient clinic started with one hospitalist, Dowlatshahi and a nurse, performing ultrasound guided paracentesis.
“Sometimes changes in operations can only be considered improvements once formally evaluated,” said Amytis Towfighi, MD, Director of Healthcare Delivery Science at SC CTSI, which focuses on improving health by improving systems of care. She introduced the clinic director—who advocated for, developed, and runs the clinic—to an experienced researcher who brought powerful evaluation tools to the partnership.
“At first, the clinic was part-time, and we were only supposed to be piloting two patients a day,” said Dowlatshahi. “But demand was so strong that we were able to get a full-time nurse practitioner to join us. And then the residents and interns were interested in rotating through with us.”
The clinic has expanded to full-time weekday hours. Dowlatshahi along with other hospitalists are providing the residents/interns with a one-week, rigorous, protocol-guided training in ultrasound-guided paracentesis and mentor them for at least five procedures.
The Southern California Clinical and Translational Science Institute (SC CTSI) and the Los Angeles County Department of Health Services (LAC DHS) funded a study to evaluate the FLASP clinic as part of a new program to support the design and implementation of interventions within DHS that will achieve the goals of quality, improved health, and patient-centered care.
“This study examined whether the FLASP clinic achieved the goal of reducing emergency department demand for paracentesis by the predominantly Latino patients served by LA General. We also examined whether the FLASP clinic was able to deliver this care safely and achieve high levels of patient satisfaction,” Turner said.
The FLASP clinic performed approximately 2,700 paracenteses over 14 months for patients with similar demographic characteristics to those undergoing paracenteses in the emergency department. Compared with 14 months before the FLASP clinic was opened, the emergency department experienced a two-thirds reduction in the rate of procedures performed among patients who were discharged home. Furthermore, the FLASP clinic met high standards for safety and received high ratings on a measure of patient satisfaction.
“This study is a model of how SC CTSI can partner with healthcare delivery institutions to do rigorous evaluations of innovations in what we call implementation research, analyzing a novel approach that helps healthcare delivery for a very important population,” Turner added.
This team also partnered on another study, exploring perspectives on the new clinic by emergency personnel and patients, accepted for publication in Digestive Diseases and Sciences. That qualitative study increased our understanding of what worked and what could have been done better to transition patients from the emergency room to FLASP.
The FLASP clinic now performs 60-80 paracenteses weekly.
“Patients said they preferred coming to our clinic because they felt safer there, and the wait time is significantly less than the emergency department,” Dowlatshahi said.
In addition, the clinic has expanded its services to include other procedures such as thoracenteses, lumbar punctures, and joint injections. The goal is to offer other clinicians and patients a safe, and accessible option for these procedures.



