USC Researchers Determine Stroke Risk in Sickle Cell Disease Patients
Novel use of imaging techniques generates surprising insights about brain blood flow that may help doctors.
In a pilot study, researchers at USC and Children's Hospital Los Angeles demonstrated that MRI techniques measuring blood flow and oxygen levels in the brain could help doctors decide when to prescribe stroke-preventing therapy in high-risk patients, while reducing use of the potentially dangerous treatments for lower-risk individuals.
"Stroke is one of the major threats to long-term physical and cognitive health and quality of life for people with sickle cell disease, but we don't fully understand the risk factors at work," said principal investigator John Wood, principal investigator at The Saban Research Institute of Children's Hospital Los Angeles (CHLA) and professor of Pediatrics and Radiology at the USC Viterbi School of Engineering. "Since we haven't been able to accurately assess stroke risk with SCD patients, it's hard to determine the best treatment path."
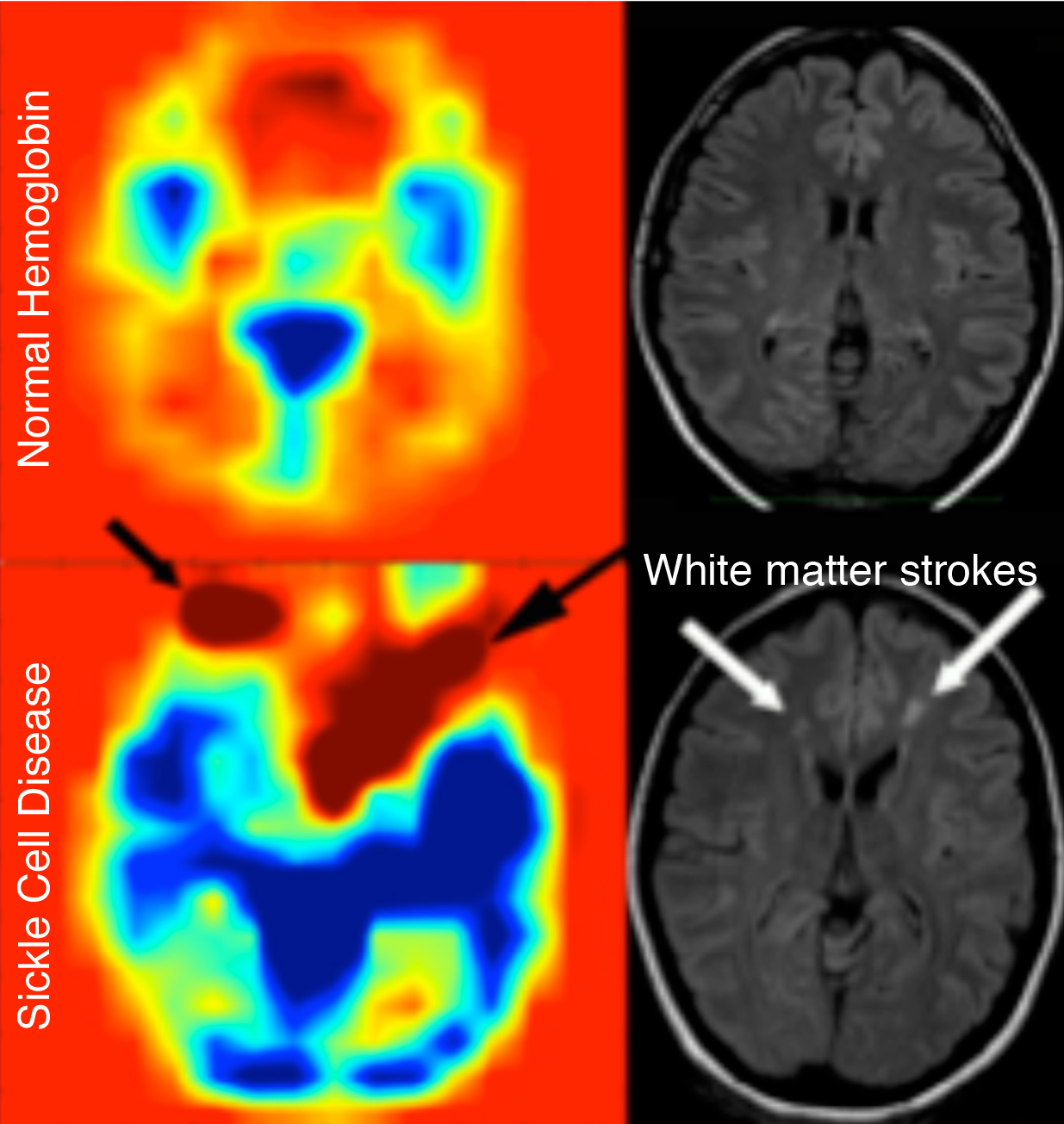
SCD is an inherited blood disorder caused by a mutation in the gene for hemoglobin, the molecule in red blood cells that carries oxygen. SCD causes these cells to assume an atypical curved shape with pointed ends that damage blood vessels, causing complications such as kidney damage and stroke. According to the Centers for Disease Control and Prevention, there are approximately 90-100,000 SCD patients in the US.
About 25 percent of people with sickle cell disease will experience a major stroke, but nearly all will have microstrokes. "Sadly, even young kids are at risk," Wood said. "About 50 percent have microstrokes by the time they're teenagers, which can impact cognitive function in school and afterwards."
Guarding against overtreatment
Currently, to predict stroke risk in SCD patients, physicians use ultrasound imaging, a method with a high rate of false-positive diagnoses that can lead to unnecessary and potentially harmful treatment.
Stroke-preventing treatment for high-risk patients involves blood transfusions, a several-hour process that must be repeated every three weeks for life. Repeated transfusions can cause allergic reaction or an overload of iron, which increases risk of heart failure, diabetes, and other conditions.
"Currently, we're over-treating 70% of the SCD population," Wood said. "We need to figure out a better way to determine which patients need aggressive therapy and eliminate unnecessary transfusions."
MRI may provide the information doctors need
The researchers found that brain blood flow in SCD patients is higher than expected. "We think that's because the disease causes over-perfusion in the brain because of damage to blood vessels," Wood said. "But we can use that to better help patients because it becomes a marker of their risk."
Researchers used two MRI techniques to measure oxygenation in their SCD patients: BOLD, which stands for Blood Oxygenation Level Dependent imaging; and TRUST, for T2 Relaxation Under Spin Tagging.
A pilot grant from the Southern California Clinical and Translational Science Institute (SC CTSI) funded the study. The work was performed at CHLA and was supported by SC CTSI’s Clinical Trials Unit at CHLA.
The research may also apply to the broader population. "We suspect the sickle cell disease process is essentially an acceleration of aging, so the same techniques may help us screen any group of patients at risk for stroke," Wood said.
The findings enabled Wood and co-investigators to obtain a $9.6 million grant from the NIH to continue clinical research with a larger number of participants. Also involved in the NIH-funded research are Thomas Coates, MD, Michael Khoo, PhD, Herbert Meiselman, ScD, and Lonnie K Zelter, MD.